Looking for a sense of perspective.....
24 February 2024
The Turning World
1 February 2024
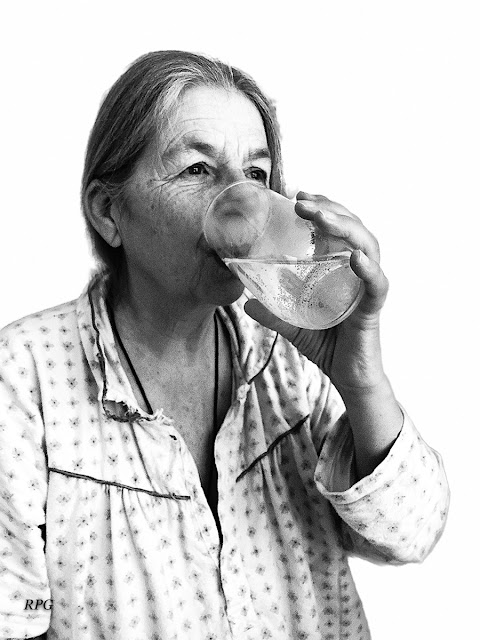
Amanda Jane Blacknell Gibbs
A nice picture of a smiley me.....
Around twelve years ago, during her menopause, Amanda suffered from an auto-immune infection and I later learned that this could well have triggered her dementia. Subsequently she began to have trouble with finding the names of things. It became frustrating and we consulted our GP, who referred her to EMDASS (Early Memory Diagnosis and Support Service - Older People's Mental Health Services in Hertfordshire, where we lived at the time.)
Amanda was visited at home and asked to complete a number of tests and then we were invited to see a doctor who specialised in ‘older people,’ (Amanda was then about 58). He decided that Amanda was suffering from Young Onset Alzheimer’s Disease, and prescribed donepezil for a year. He told me that the problem I had, was that she might live for twenty years.....
I made a note that day, Friday 15th October, 2012.
Diagnosis – Amanda has Early Onset Alzheimer’s. She returns to work. Later she says if she had not got her faith that she is being taken care of she would have been in tears all day.
I think we are both in shock. The details are unimportant. The fact is this is a ‘life sentence’ and may also affect the girls: their future health may be shadowed by this.
In 2014, although Amanda was still working as a Teaching Assistant in a Preparatory School, and was driving and, to all intents and purposes, living a normal life, it was clear that she was having serious problems with words and I was not convinced that she was suffering from Alzheimer’s. The doctor referred her to a neurologist who arranged for her to have an MRI scan. This showed asymmetric (left) temporal lobe atrophy with prominent inferior loss and relative preservation of the left superior temporal gyrus, in keeping with a diagnosis of Semantic Dementia. Following this, and further exhausting testing, including a whole day at the Royal Free Hospital in Hampstead, the doctor insisted that Amanda should discuss her diagnosis with her Headmistress.
Prior to that meeting in November 2014, Amanda made a few notes which she gave to me at the time:
· I have recently had to have a Head Scan at the Hospital and then some further testing. I have recently been told that my left side is a little bit narrow! And I have been told I have ‘semantic dementia.’
· I feel very well!
· I did complete my First Aid Course Training!
· I have no illness or difficulty.
· I read Bible lessons every day and know that God is with us all the time!
· I do take some medication (Donepezil) but I have no problems and am very happy to be continuing working here as a T.A. and doing Pre-Prep After School Care.
· I did mention that I thought I would be retiring at the end of the year, which I will then do.
Amanda continued working at the school until the summer of 2015, when, reluctantly (she would have no pension for some years, and she loved her work and her colleagues and the children) she took early retirement.
Amanda built up a series of pictorial aides. She cut pictures from magazines and papers and stuck them on sheets of A4 paper, organised into logical groups. So, for example, she had pages of farm animals, then pages of wild animals, then of birds. She had pictures of her friends, with their families and details, to remind her if they called. She had favourite foods so that she could interpret menus in restaurants. And then she had maps of where we had been on holidays, so that if someone came to see her, she could get out the map and show pictures of places.
In addition to this, she began meticulously labelling items around her – her bedside clock, for example, had a little label saying “clock” stuck on the back. She had made explanatory cards, which showed her what the things in the bathroom were for: for example, “Passion body spray – in summer times I have to add, to clean this up, to keep it well,” with a little drawing of a girl with her arms uplifted; an interdental brush has the label, “This is useful for my teeth!” and one sheet is headed, “Things to take abroad!” and has neat little sketches accompanied by notes. One picture is a self-portrait with an arrow indicating “This is my eyebrows (and I clear these things each day!)”
A doctor at The National Hospital for Neurology and Neurosurgery in London monitored Amanda. We went to see him every six months at his Cognitive Disorders Clinic and then in 2017, in the autumn, following repeated advice from that doctor, Amanda had an assessment of her driving. That year she was deemed to be safe on the road and so kept her licence, and the independence this accorded her. She had been driving for forty-five years and she loved her little car but in November 2018 she had to be reassessed and this time the assessors had to take her licence. Amanda could not grasp this and for perhaps the first time in our married life I found her becoming emotionally upset.
She became convinced she could buy another car, and she would get me to take her to car dealers, carrying a bag containing several hundred pounds cash and once she got herself to a Jaguar Salesroom and the concerned staff called the police to bring her home.
On October 14th 2019, we saw another doctor in the London clinic, who reported that Amanda:
remains in good health and positive spirits.
However, she has very little comprehension now and [her] verbal output is limited to stock phrases.
Overall, it is clear that things are progressing slowly. This is naturally stressful; however, Mr Gibbs and the family are obviously supporting [her] very well......
In many ways, our life could have been worse. Amanda needed attention, and was no longer able to cook, but she could dress herself and could take herself to the toilet and, providing I monitored the temperature, have a bath. She watched television, and we still went swimming twice a week and I would take her for a country walk every morning, rain or shine. I managed to employ agency carers who gave me a little respite. It wasn’t as I had hoped our retirements would be, but it could have been much worse.
For various reasons, one of which was the need to have more space for family and carers to stay with us, I arranged to move, and in January 2021, just before my seventieth birthday, with the pandemic still keeping things closed, we moved to Snettisham, a village in Norfolk.
Amanda was very confused, and for what seemed an eternity she wouldn’t settle. She had her bag with her precious things (glasses, iPad, phone and wallet) and she sat at the foot of the stairs with her coat on, sporadically getting up to try the door.
I fairly soon managed to engage some help from agency carers to give me a little time to devote to sorting the house out. But Amanda was not settling and we had to resort to diazepam, which was a mistake, as it caused her to have a horrendous accident in her bathroom. Medical intervention changed diazepam to lorazepam to help calm her, and then another doctor prescribed memantine. Fortunately I was able to employ two independent carers as well as the agency staff, which helped enormously.
By November Amanda had become doubly incontinent and was in need of constant supervision. She could no longer communicate, and she was getting up in the night and sometimes falling. A doctor managed to prescribe her melatonin, which did help, but then the prescription was disallowed as NICE had not licensed it (although I did manage to get it legally from America, Australia and Italy).
Memantine, risperidone and zopiclone with supper then to bed by 6.30. Reappeared at 7.00 ish so gave her a drink with a second zopiclone. Changed pants and put her back to bed...... Half an hour later going downstairs again (unsteady). Gave her water and helped her back to bed (very unsteady). Then ok til 4.37 am, down for water, changed pants. Then up again at 5.13 – made it back upstairs unaided. 7.30 am fell getting out of bed.
Reluctantly, in September 2022, I arranged for Amanda to become a resident of a nearby Care Home. I felt horribly guilty for letting Amanda go, but, as friends and experts advised me, I needed to try and reclaim a little of my own life, while that lasted.
Over a year later, we had our routines and I was still taking her out in the car, but she could no longer walk, nor talk, nor feed herself and she was often very sleepy. I lift her into a wheelchair and we take fresh air, but otherwise she is simply wheeled from bed to breakfast to the lounge to lunch to the lounge to supper to bed. She is cared for and cleaned but it’s not great....
I have a sheet of A4 paper covered in Amanda’s neat handwriting in black ink. It is undated, but I know she wrote it many years ago. She has put her initials in the margin – AJBG and written beside that “ABeeGee!”
If (& when!) it’s time for my funeral don’t really like that word so could it be a celebration of life around here please, there are a few suggestions which might be helpful to whoever has to put it all together (Good luck to you!!)
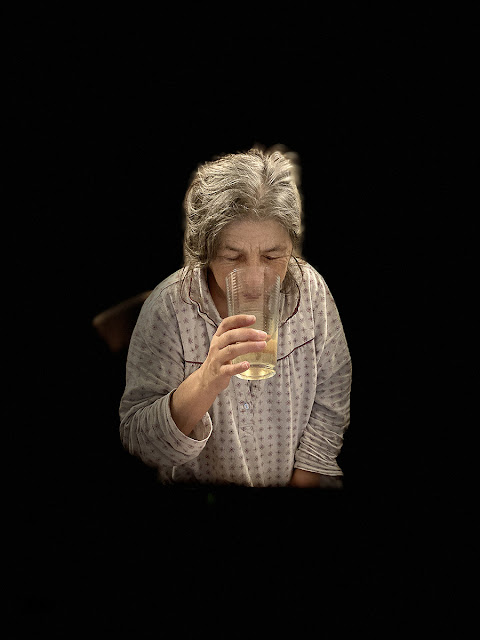
A nice picture of a smiley me would be good.
Lots of thanks for such lovely times, so much fun experienced, very dear loving family (including furry members) & very kind friends & colleagues throughout life. Wonderful times in Italy & here!
Note that I will have moved on somewhere & look forward to seeing you all there at some time later!
(Dear family....) Try not to feel sad, but happy & grateful for all we’ve shared & learned together & know that God is always guiding & taking care of everyone & showing everyone where to go at the right time & sending love
Everlasting arms of love are beneath, around, above
God it is who bears us on, His, the arms we lean upon
The joy that none can take away, is ours. We walk with love today.
Some nice happy hymns/songs
Lovely Italian music at the start – don’t like coffins coming in in silence, and also at the end.
The lord’s prayer somewhere.
Whatever else suits you.
Try to make it a good, happy, warm, time for support for those who might need it.
In loving memory of my dear wife
Amanda Jane Blacknell Gibbs
March 5th 1954
to
February 1st 2024
30 June 2022
An open letter to the Health Secretary
Secretary of State for Health and Social Care,
House of Commons,
London,
SW1A OAA
30 June 2022
Dear Mr Javid,
I am writing to you concerning an issue which is adversely affecting my wife’s (and indirectly my) health. In advance I apologise for the length of this, but I feel it necessary to present you with the full story, partly because we will not be alone in this.
My wife, Amanda, who is now 68 years old, was diagnosed with dementia over ten years ago. Initially the diagnosis was early onset Alzheimer’s disease, and she was prescribed Donepezil for a year. I was not convinced by this diagnosis, however, and so, after extensive further testing, a brain scan, and the involvement of a neurologist, the diagnosis was corrected to Frontotemporal Dementia (Semantic Variant) a rare form of dementia which has an approximate life expectancy of twice that of Alzheimer’s, and for which there is no cure nor officially authorised medication.
For several years she has been seen by Professor Jonathan Schott, Professor of Neurology at the Dementia Research Centre, UCL Institute of Neurology and Honorary consultant neurologist at the National Hospital for Neurology and Neurosurgery, Queen Square. Professor Schott has maintained contact with me as Amanda’s husband and principal carer (with LPA) over the years, though Amanda is no longer capable of attending his clinic nor of understanding nor communicating as the disease has robbed her entirely of speech.
For the record we moved from Hertfordshire to Norfolk in January 2021, partly to give us more space to accommodate our daughters and other carers who may need to stay overnight. Since the move Amanda’s condition has deteriorated (for example she is now entirely dependent on myself or carers for everything, from washing and dressing - she is doubly incontinent - to eating and drinking and going out for walks). Since that move, we have had involvement from our new GP surgery, as well as Older Peoples Memory Assessment Team at Chatterton House, Adult Community Mental Health Service West and South Norfolk, who, in February 2021, recommended trialling Memantine Hydrochloride, which she now takes at 20mg a day, which may have helped keep her calmer as she was very disturbed by our move. We have also had help from Adult Social Services, and have been visited by NHS Occupational Therapists who have provided some devices which help with Amanda’s security in the house.
However, and, after that preamble, this is the heart of the matter, Amanda has developed a tendency to get up and walk about at night, taking a risk in going downstairs as many as six times a night. Generally, I am able to help her and to give her a drink of water and take her to the toilet, but on occasions she has fallen out of bed, or on the stairs, and quite often she gets stuck at the top of the stairs if I am not there. Sleep disturbance is common among people with dementia and the impact for patients and their families is significant, and there are no easy solutions.
The effect of this is that she is not getting enough rest, but this is also having a negative effect on my ability to care for her.
In order to calm her and to help her settle at night, she was prescribed Risperidone (0.25 mg), an antipsychotic which is used to treat Schizophrenia, Mania, and aggression in people with Alzheimer’s dementia.
As an additional attempt to get her to sleep better she was prescribed Melatonin (Mylan) 2 mg prolonged-release tablets. The active ingredient of these tablets is melatonin which belongs to a natural group of hormones produced by the body. This hormone synchronizes the body’s biological day-and-night rhythm. Although Amanda would still wake during the night (usually either because of incontinence or because of thirst) the effect of this prescription seemed entirely positive with no noticeable side effects.
However, when I requested a renewed prescription, this was denied, apparently because it should only be prescribed in hospitals(?) I questioned this but was told that there is some controlling body within the NHS, possibly within Norfolk, which will not allow the prescription of Melatonin by GP practices.
The result of this was that the only viable alternative was deemed to be the Z drugs, such as Zolpidem and Zopiclone. And so, we started to give her one or two Zopiclone 3.75 mg tablets at night. This is a hypnotic or sleeping tablet. What I did not know was that this drug should not be taken with antipsychotics such as Risperidone, one of the recognised side effects of which is signs of a stroke, such as a sudden weakness or numbness in the face, arms or legs, especially on one side. Amanda did indeed appear to be affected in this way (though she cannot articulate her feelings) and one morning in May I had to call an ambulance as I feared she might have had a stroke. After discussions with various medical professionals on that occasion we agreed to stop giving her Risperidone and she recovered from that incident. In the meantime, it seemed that after a few days of taking Zopiclone it may have accumulated in her body, and the recognised side-effects of reduced alertness, dizziness, confusion, loss of co-ordination, muscle weakness, restlessness, accompanied by several incidents in which she fell, all appeared to be present (though again there is no way of consulting Amanda about her feelings as she is incapable of communication).
We have stopped the Risperidone. We have since stopped Zopiclone. We are not allowed to have a prescription for Melatonin. And apparently there are no other viable alternatives.
So, what I am writing to you about is to enquire as to why we cannot have Melatonin on the NHS? It is available over the counter in the United States and Australia, and it is available online in this country. Melatonin is a naturally occurring hormone produced by the pineal gland and is structurally related to serotonin. Physiologically, melatonin secretion increases soon after the onset of darkness, peaks at 2-4 am and diminishes during the second half of the night. Melatonin is associated with the control of circadian rhythms and entrainment to the light-dark cycle. It is also associated with a hypnotic effect and increased propensity for sleep.
However, I note that there has been a case in the Court of Appeal concerning the production of Melatonin, as a company called Neurim Pharmaceuticals is the registered proprietor of EP 1 441 702 (the Patent), which expires on 12 August 2022. Could it possibly be that the NHS is caught up in the business affairs of Mylan and Neurim, and that as a result my wife and many others are being denied a relatively harmless pharmaceutical product?
I appreciate that even if Melatonin were to be prescribed for Amanda, it may not be suitable for long-term use, and I also know that it is not a magic bullet which will enable me to sleep undisturbed throughout every night. But Amanda is dying and I am endeavouring to keep her in her home for as long as I can protect and care for her. Strong sleeping pills known as ‘Z-drugs’ are linked with an increased risk of falls, fractures and stroke among people with dementia – according to research from the University of East Anglia, involving the University of Exeter. Prof Chris Fox, from UEA’s Norwich Medical School, said: As many as 90 per cent of people with dementia suffer sleep disturbances and it has a big impact on their mental and physical health, as well as that of their carers. To date there are no proven effective treatments available, however people with dementia are often prescribed Z-drugs (zopiclone, zaleplon, and zolpidem). But a new study reveals that stronger doses of these drugs are linked with an increased risk of adverse effects.
And, as described above, Risperidone is not the answer either.
So, please could you look into this issue? Perhaps with the expiry of Neurim’s patent in August other companies will be able to produce melatonin tablets at reduced costs and perhaps then GPs will be able to prescribe it, or perhaps even it will become available over the counter in Pharmacies? It would be good to have a little light thrown on this and to feel that the miserable world of sufferers from dementia and their families and carers is not being ignored or made more difficult by business concerns.
Thank you for your attention,
Yours sincerely,
Richard Gibbs
cc: James Wild MP, Professor Jonathan Schott, Heacham Group Practice, Chatterton House
1 January 2022
A New Year message from Amanda
Keep Smiling Through.....
With love,
Richard